It’s on everybody’s lips: the Quebec population is aging.
According to the Institut de la statistique du Québec, a third of Quebecers will be aged 65 or more in 2061.
And more a person ages, greater is the risk of developing a neurocognitive illness.
Without a doubt, these stakes will solicit greatly our health system.
In this context, will the Quebec aid system perform well? Would we benefit from taking inspiration from what is being done elsewhere in the world? In France, for example, where the health expenses are higher than in Quebec.
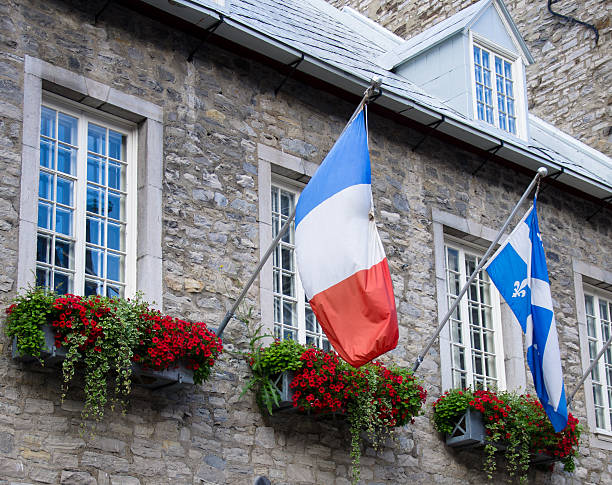
In this article, I have chosen to compare the aid structures in France and Quebec, structures that are precisely for persons who have a neurocognitive disease.
In France

The departments
In France, the social aspects and the assistance to the elderly persons is managed by the departments. Each region of the French territory (equivalent of Canadian provinces) is divided in several departments.
Centres locaux d'information et de coordination (CLIC)
Inside each department, you will find the CLIC. They are organizations that give the first information concerning the management of neurocognitive diseases. They explain the different types of support, the contacts to have and the specialists to meet. They determine if there is a need to open a file for persons with loss of autonomy. There are more than 600 CLIC in France, that can have a different name in each department.
Méthode d’action pour l’intégration des services d’aide et de soins dans le champ de l’autonomie (MAIA)
The MAIA takes over from the CLIC if there is a need to open a file for a person with loss of autonomy. The MAIA gives to the patient a case manager. The role of the case manager is to coordinate the actions between all the persons that are involved in the protection of the patient, and this, at every level: financial, legal and medical.
It’s the case manager that ensures the coordination between the doctors, the patients, the caregivers and other related organizations. For example, it is the case manager who can request assistance with household or body care (Allocation personalisée d'autonomie).
Moreover, the department sends an expert doctor to evaluate the level of autonomy of the patient and consults the MAIA before deciding what level of financial aid to grant.
The EHPAD
When the patient cannot stay at home, he/she is referred to the EHPAD (Établissements d’hébergement pour personnes âgées dépendants). These are nursing homes offering room reception. The EHPAD are for elderly persons of over 60 years old that need help and care on a daily basis. The EHPAD can be financed by the public sector or the private sector.
Assistance for the caregiver
Concerning the help for the caregivers, there are associations like France Alzheimer that organize training for the caregivers.
France can also count on associative-type structures such as support groups and discussion groups, where caregivers can meet other caregivers in order to discuss various everyday tips.
Caregiver leave
Since December 2020, the caregiver can benefit from caregiver leave. This leave allows you to stop working to take care of a person with a loss of autonomy. It is accessible under certain conditions (family or close bond with the person assisted) and lasts three months (can be renewed for one year). Caregiver leave is not paid by the employer. However, the employee receives a daily caregiver allowance (43.83 euros for a person in a couple and 52.08 euros for a person living alone. The amounts of the allowance are readjusted each year on April 1st.er avril.)

The strong points of the French system
The strong points of the French system are the accompaniement and the advices given by the CLIC and the MAIA. It is precious advices and the health care workers have real human values such as respect, fairness, empathy, that should be recognized and valued.
The weak points of the French system
The weak points of the French system are, among others, the lack of staff allocated to CLIC and MAIA. They do a lot with little time and money. And second, the general practitioner does not sufficiently fulfill his role of medical coordinator with the various stakeholders.
In Quebec

In Quebec, the help given to the elderly is managed by the government of Quebec.
The CLSC
Relatives of people with neurocognitive disease must first refer to the CLSC for support.
It should be noted that the CLSC offer current health and social services, medical, rehabilitation and public health services. They are part of the CIUSSS (Integrated University Health and Social Services Center) with hospitals and CHSLD.
There are more than 160 CLSC in Quebec.
The soutien à domicile
Within the CLSC, we find programs of soutien à domicile (SAD). They ensure the support at home so that the person who has dementia can live the longest time possible at home.
SAD are offered in partnership with community organizations (eg Support for Caregivers), social economy enterprises in domestic help (EESAD) and private businesses in order to meet the needs of the user.
The CHSLD
When home support has become impossible and the affected person has a severe loss of autonomy, relatives most often place him/her in a CHSLD. This structure provides medical and nursing follow-up, medication management and surveillance. The workers assist people in their daily activities and their mobility.
Alzheimer home
In Quebec, there are also Alzheimer houses, which are inspired by Holland. These homes welcome residents with Alzheimer's disease in a supervised and flexible environment. These are living environments with a human dimension, where there are few residents and where workers spend quality time with users.
Fédération québécoise des Sociétés Alzheimer
The Fédération québécoise des Sociétés Alzheimer (FQSA) is another resource on which people with Alzheimer's disease and their families can rely. The FQSA also contributes to biomedical research into the causes and treatments of Alzheimer's disease. She educates the general public about this disease.
Compassion benefits
In Quebec, workers can receive compassionate care benefits (up to 26 weeks). These benefits apply to any worker who takes care of a loved one at the end of their life.
However, there are no comparable measures for people who are not working (eg retirees).
The strong points of the Quebec system
The Quebec system is based on a holistic approach, centered on patients and not on their illnesses. Patients and their caregivers are encouraged to participate throughout the care process, with respect for their dignity. The care provided throughout the disease continuum is adapted to changing needs, which requires the involvement of various first, second and third line workers.
The weak points of the Quebec system
On the other hand, it is sometimes difficult to rely on regular CLSC staff (they are on study leave, statutory holidays, training session, sick leave, vacation). Bureaucratic and financially constrained, the Quebec system is characterized by long waiting lists for clinical memory assessments, diagnostic delays and late start-ups of home care.
Conclusion: comparison of French and Quebec aid structures
In terms of France-Quebec similarities, we can cite a localized range of services as well as stakeholders with real human values and who do their best with few resources. Both France and Quebec are facing a labor shortage.
In terms of differences, the French aid structures are a little more complex (CLIC, MAIA, medical expert) than in Quebec, where care is provided through the family doctor and the CLSC. In addition, French caregiver leave concerns anyone with a loss of autonomy, while in Quebec, compassionate care benefits concern a loved one at the end of their life. Finally, the waiting lists for services are longer in Quebec than in France.
Overall, the French and Quebec aid systems are efficient (France does a little better than Quebec) but they could certainly be improved. The ideal would be a team that take care of patients 24 hours a day for free. Anyway, compared to other countries, French and Quebec patients are all blessed in terms of support structures.
Howdy! Someone in my Myspace group shared this website with us so I came to give it a look.
I’m definitely loving the information. I’m book-marking and will be
tweeting this to my followers! Superb blog and excellent style and design.
Hello there! Would you mind if I share your blog with my facebook group?
There’s a lot of people that I think would really appreciate your content.
Please let me know. Thank you